Delayed sleep phase this month and chronotherapy which sounds like quite an undertaking. Also a link to a new parent’s guide to picking up and talking about sexual abuse, links to handy recent uploads to the site, the BSACI guideline on allergic rhinitis and more banging on about vitamin D supplementation – please.
Category Archives: For Emergency Departments
Dr Anshoo Sahota’s personalised eczema plans
Anshoo Sahota is a dermatologist at Whipps Cross Hospital (Barts Health) who has devised this personal eczema management plan with drop down menus you choose from before printing them out for your patient to take home with them. The paediatric one has pretty pictures on but is the same otherwise. Please note that they don’t download properly on iPads.
Dr Noimark’s allergy management plans
Lee Noimark is a paediatric allergist at the Royal London Hospital. He and his team put these allergy action plans together. Print them out for your patients to give to nursery or school in the event of an allergic reaction. The labels are self explanatory:
Allergy Action Plan (mild-moderate)
Allergy Action Plan (mild-moderate with asthma)
Allergy Action Plan (severe with asthma)
February 2013 uploaded!
A timely reminder of an albeit old guideline on otitis media this month, continuation of our minor injuries series and introduction to a new series on sleep disorders. Also a link to a new Whipps “1st afebrile fit” guideline and a bit of background on hypospadias.
January 2013 – Happy New Year!
I was a bit overloaded in December and couldn’t manage to get a newsletter out. The nurses in my own ED noticed but I don’t think anyone else was particularly bothered! Hope the Christmas break went well for everyone. January 2013 brings some more on speech development, a reminder of the BTS 2008 guideline on cough, another plug for vitamin supplementation and part 2 of Jess Spedding’s minor injuries series. Do leave comments below.
Minor injuries part 2
With thanks to Dr Jess Spedding for the continuation of her minor injuries series….
Minor Injuries Series, part 2: The Elbow Xray and Supracondylar fracture:
The elbow xray typically strikes fear into the heart of clinicians as there are so many centres of ossification which appear at different stages of a
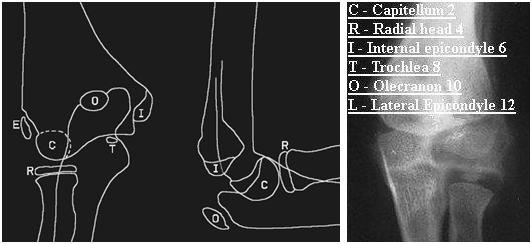
child’s development and can quite easily be mistaken for bony injury. Remember that the smooth rounded appearance of a centre of ossification does not often mimic the typically sharp edges of a new fracture fragment, but even saying this, distinction can be very difficult. If you have the CRITOL (or CRITOE) acronym in your mind, it will help you to interpret the xray with a sensible approach. The image below highlights each of the six ossification centres with the typical age of the child when each centre appears:
Note: Lateral / External epicondyle are interchangeable terms, giving either CRITOL or CRITOE
Work through in order the centres of ossification – each may appear at slightly different ages in different children, but the sequence in which they
appear should always be C,R,I,T,O,L. For example in a 6 year old you would not expect the lateral condyle to have appeared yet, so if there is a bony fragment at that site, it is suggestive of a fracture.
Supracondylar Fractures:
The supracondylar fracture (of the distal humerus) is the most common upper limb fracture in young school age children. It presents almost always as
a FOOSH (fall on the outstretched hand). They are likely to be in a lot of pain, and may need strong analgesia and immobilisation (with a splint or
sling) before assessment is possible. (A good example of a strong, rapid acting, well tolerated analgesic that can be used in the Emergency Department is intranasal diamorhpine, which is made up with saline into a small volume of fluid and then given as nose drops with a syringe.)
You may well see bruising and swelling around the elbow, with tenderness around the distal humerus, but remember to check the whole limb including
clavicle (and the whole of their body if the mechanism of injury could have caused other serious injuries!)
The elbow contains numerous important neurovascular structures – your assessment must document presence of radial pulse, capillary refill time in
fingertips and function of ulnar, median and radial nerves (not possible formally in younger children, so watch to see if they will hold a toy or parents hand
and be suspicious if the xray shows a displaced fracture). Any concerns about neurovascular compromise require the fracture to be urgently reduced, either by the Emergency Department team or referral to Orthopaedics. This initial reduction is to relieve mechanical pressure of displaced bony fragments on the
neurovascular structures and will not provide the stability required for neatly aligned healing, so a trip to theatre for fixation will happen soon after.
A common classification system for supracondylar fractures is the Gartland classification. In this there are three categories of supracondylar fractures based on their radiological appearance on the lateral elbow view:
1: undisplaced – recognised as clinical suspicion plus xray evidence of fluid in the elbow joint elbow (as demonstrated by a raised anterior fat pad or
the presence of a posterior fat pad) and possibly loss of anterior humeral line (normal is when line along anterior humerus intersects middle third of
capitellum)

2. visible fracture which is hinging on the posterior edge

3. totally displaced
Type 1 can usually be managed conservatively with an above elbow cast and sling, whilst 2 and 3 require operative fixation.
All should be followed up by Orthopaedics in fracture clinic – typical progress is evidence of union at 4 weeks, and then the patient is encouraged to
gradually do away with the sling, to allow mobilisation without too much discomfort.
A rare but debilitating late complication of supracondylar fractures is Volkmann’s ischaemic contracture (when the brachial artery is damaged and months later the patient develops clawing of the thumb and fingers and forearm wasting).
November 2012 published!
The common assessment framework triangle for assessing children in need this month with some tips on how to press the right buttons with children’s social care referrals. Also a bit on stabilisation and transfer for the ED teams, a reminder not to use 0.18% saline and the start of a minor injuries series. Talipes for the GPs and paediatricians among you.
Minor injuries introduction
Minor injuries Series: Episode 1 with thanks to Dr Jessica Spedding, PEM trainee, Royal London Hospital, UK
Introduction to minor injuries:
Minor injuries in children are common and mostly self limiting soft tissue injuries that heal with time. Some injuries are particular to paediatrics (pulled elbow) and others are simply much more common in children than adults (supracondylar fracture). Another consideration specific to children is consideration of growth plate involvement, which if does not heal in a good position could lead to asymmetry and growth problems. Injuries involving the growth plate are graded as Salter-Harris 1,2,3,4, or 5 and they will be discussed in more detail in a future episode of this minor injuries series.
Your assessment:
You need a systematic approach that assesses for important injuries that need specific management. Your
assessment must always include consideration of non accidental injury (NAI). A sensible approach would include:
– Is the mechanism of injury described consistent with the injury sustained?
– Has the child reached the appropriate stage of development to have sustained the injury in the way described?
– Is there any delay in presentation?
– Has the child (or siblings) presented numerous times before with injuries?
– There is an excellent set of pamphlets that give evidence based guidance on when injuries point to abuse – go to www.core-info.co.uk or look out for the summaries on Paediatric Pearls
Upper limb injuries:
You may have come across the acronym FOOSH. This is a Fall On the Out-Stretched Hand. This mechanism is the natural response to a fall – in order to protect our head and trunk, the reflex is to put our arms out to break our fall. This mechanism causes a number of different injuries, each more prevalent in different age groups (but common in other age groups too). Roughly speaking these could be sequenced as follows:
Age 1-3: distal radius fracture (usually greenstick or torus) or middle third clavicle fracture
Age 4-8: supracondylar fracture (varying degrees of severity, some of which require operative fixation)
Age 9-adulthood: distal radius fracture or scaphoid fracture
However one must still examine unclothed the whole limb to be sure that all sites of injury have been located. In the upper limb this would be from
fingers to shoulder, clavicle and possibly neck, in the lower limb this would be from toes to hips but also checking the pelvis and lower spine.
The first chapter in this series looks at a common elbow problem:
Pulled elbow: (see also http://www.paediatricpearls.co.uk/2012/02/pulled-elbow/)
 Proper name – radial head subluxation, mechanism is usually a sudden pulling of the child by their hand (such as to stop them running into the road or swinging a child in play), child presents having cried initially, but soon settles but refuses to use the arm, holding it slightly flexed at the elbow with the arm by their side. When you go to assess them they have no swelling or bruising or distal neurovascular compromise, but are very apprehensive about you trying to bend or pronate/supinate the elbow. In up to half of cases there may not be a “pull” mechanism in which case be more cautious in assuming the diagnosis. Don’t forget a clavicle fracture may present this way. If you feel sure the diagnosis is pulled elbow, attempt a reduction as follows:
Proper name – radial head subluxation, mechanism is usually a sudden pulling of the child by their hand (such as to stop them running into the road or swinging a child in play), child presents having cried initially, but soon settles but refuses to use the arm, holding it slightly flexed at the elbow with the arm by their side. When you go to assess them they have no swelling or bruising or distal neurovascular compromise, but are very apprehensive about you trying to bend or pronate/supinate the elbow. In up to half of cases there may not be a “pull” mechanism in which case be more cautious in assuming the diagnosis. Don’t forget a clavicle fracture may present this way. If you feel sure the diagnosis is pulled elbow, attempt a reduction as follows:
 Hold their hand as though you were going to shake hands, with your other hand gently cupping underneath the elbow, with elbow partially flexed, then firmly pronate (rotate to palm up position). You should feel the clunk of a reduction, but if not, try a firm supination (back to palm down position). Ideally do this half an hour after some analgesia. If you do not feel a clunk it is probably not reduced but either way stop after two attempts, and then allow the child to be somewhere relaxing and ask their parent to let you know if they start playing – if reduced most will soon realise the pain with movement has gone and start playing normally within a few minutes. If not reassess and consider a differential diagnosis which may include referral for xray.
Hold their hand as though you were going to shake hands, with your other hand gently cupping underneath the elbow, with elbow partially flexed, then firmly pronate (rotate to palm up position). You should feel the clunk of a reduction, but if not, try a firm supination (back to palm down position). Ideally do this half an hour after some analgesia. If you do not feel a clunk it is probably not reduced but either way stop after two attempts, and then allow the child to be somewhere relaxing and ask their parent to let you know if they start playing – if reduced most will soon realise the pain with movement has gone and start playing normally within a few minutes. If not reassess and consider a differential diagnosis which may include referral for xray.
NICE headaches
- worsening headache with fever
- sudden-onset headache reaching maximum intensity within 5 minutes
- new-onset neurological deficit
- new-onset cognitive dysfunction
- change in personality
- impaired level of consciousness
- recent (typically within the past 3 months) head trauma
- headache triggered by cough, valsalva (trying to breathe out with nose and mouth blocked) or sneeze
- headache triggered by exercise
- orthostatic headache (headache that changes with posture)
- symptoms suggestive of giant cell arteritis
- symptoms and signs of acute narrow-angle glaucoma
- a substantial change in the characteristics of their headache.
- compromised immunity, caused, for example, by HIV or immunosuppressive drugs
- age under 20 years and a history of malignancy
- a history of malignancy known to metastasise to the brain
- vomiting without other obvious cause.
- frequency, duration and severity of headaches
- any associated symptoms
- all prescribed and over the counter medications taken to relieve headaches
- possible precipitants
- relationship of headaches to menstruation.
| Headache feature | Tension-type headache | Migraine (with or without aura) | Cluster headache | |||
| Pain location1 | Bilateral | Unilateral or bilateral | Unilateral (around the eye, above the eye and along the side of the head/face) |
|||
| Pain quality | Pressing/tightening (non-pulsating) | Pulsating (throbbing or banging in young people aged 12–17 years) | Variable (can be sharp, boring, burning, throbbing or tightening) | |||
| Pain intensity | Mild or moderate | Moderate or severe | Severe or very severe | |||
| Effect on activities | Not aggravated by routine activities of daily living | Aggravated by, or causes avoidance of, routine activities of daily living | Restlessness or agitation | |||
| Other symptoms | None | Unusual sensitivity to light and/or sound or nausea and/or vomiting Aura2 Symptoms can occur with or without headache and:
Typical aura symptoms include visual symptoms such as flickering lights,
spots or lines and/or partial loss of vision; sensory symptoms such as numbness and/or pins and needles; and/or speech disturbance. |
On the same side as the headache:
|
|||
| Duration of headache | 30 minutes–continuous | 4–72 hours in adults 1–72 hours in young people aged 12–17 years |
15–180 minutes | |||
| Frequency of headache | < 15 days per month | ≥ 15 days per month for more than 3 months | < 15 days per month | ≥ 15 days per month for more than 3 months | 1 every other day to 8 per day3, with remission4 > 1 month |
1 every other day to 8 per day3,
with a continuous remission4 <1 month
in a
12-month period
|
| Diagnosis | Episodic
tension-type headache
|
Chronic tension-type headache5 | Episodic migraine (with or without aura) | Chronic migraine6 (with or without aura) | Episodic cluster headache | Chronic cluster headache |
| 1 Headache pain can be felt in the head, face or neck. 2 See recommendations 1.2.2, 1.2.3 and 1.2.4 for further information on diagnosis of migraine with aura. 3 The frequency of recurrent headaches during a cluster headache bout. 4 The pain-free period between cluster headache bouts. 5 Chronic migraine and chronic tension-type headache commonly overlap. If there are any features of migraine, diagnose chronic migraine. 6 NICE has developed technology appraisal guidance on Botulinum toxin type A for the prevention of headaches in adults with chronic migraine (headaches on at least 15 days per month of which at least 8 days are with migraine). |
||||||
October 2012 ready to go!
Coins, magnets and batteries on the menu this month as well as some more cows milk protein allergy resources. A reminder about child developmental milestones courtesy of one of our medical students and NICE on headaches. Do leave comments!