Some useful bits and pieces this month, I hope. Pointers to a CPD opportunity on autism and eating disorders and October’s relevant awareness day for children with developmental language disorder. Also the updated Vitamin D guideline.
Some useful bits and pieces this month, I hope. Pointers to a CPD opportunity on autism and eating disorders and October’s relevant awareness day for children with developmental language disorder. Also the updated Vitamin D guideline.
Burns this month – with much discussion amongst the editorial group prior to publication. There are lots of different children’s burns protocols it transpires. RCEM’s is not aligned with the London and South East Burns Network’s. The message is “use your own burns referral unit’s guideline”. The other important message about burns is watch out for NAI but, even if the burn is accidental, refer all children to their health visitor as HVs in the UK are responsible for talking to families about safety in the home.
Also, complications of Kawasaki Disease, ADHD and the updated MAP guideline (managing cows milk allergy in primary care) which emphasises that 98% of crying babies do not have CMPA. Do leave comments below.
with thanks to Dr Monika Bajaj, neurodevelopmental paediatrician practising privately in east London.
ADHD is a chronic life long disorder of self-regulation with symptoms persisting in >70-80% adolescents and >50% adults.
It is real disorder with real long-term risks, just to quote a few impacts….
Red Flags:
ADHD is usually diagnosed after the age of 6 years to allow for the child to mature. Almost all children have times when their behaviour seems unacceptable and age inappropriate. However, when behaviours happen many times a week or daily, ADHD ought to be looked for. NICE guidance allows children to be treated after the age of 5 years and medication makes a huge and quick difference along with psychoeducation and behavioural management.
Resources: The Canadian ADHD Resource Alliance (www.caddra.ca is an excellent resource for professionals with free downloads).
US guidelines have recently changed to allow treatment of some 4 year olds with debilitating features of ADHD (https://www.healthychildren.org/English/news/Pages/Practice -Guideline-for-the-Diagnosis-Evaluation-and-Treatment-of- ADHD.aspx)
UK support group: https://www.borntobeadhd.co.uk/
Cyclical vomiting this month as the message from the front line, BESS as a learning point for those monitoring the size of an infant’s head, milia also for the babies and the perennial problem of whether or not montelukast works to control episodic wheeze. Do leave comments below:
NICE on faltering growth this month, paediatric stroke, a reminder of the new epilepsy classification and a contribution from the safeguarding team on what constitutes a “legal high”? Do leave comments below:
Retinoblastoma mnemonic this month. Plus information on lower sugar content recipes for the reintroduction of cows milk into a child’s diet, labial adhesions, 6 in 1 vaccine and don’t miss infantile spasms as early treatment improves overall prognosis. Do leave comments below.
With thanks to Geoff Ferguson, Director of the Parent Infant Centre (www.infantmentalhealth.com) for the following explanation of the Acquarone scales:
The Acquarone Detection Scales for Early Relationships are observational scales that provide a powerful tool for assessing an infant’s capacity to form relationships and a mother’s ability to respond to her infant. The scales have been developed during several decades of clinical practice by Dr Stella Acquarone, who is also the author of several books on infant development and parent infant psychotherapy and Principal of the Parent Infant Clinic. The Parent Infant Clinic is a private service but does have some subsidised places for families with limited financial resources.
There are two scales, a 25 item scale for observations of the infant and a 13 item scale for observations of the mother. In each case observations are divided into four domains: interpersonal, sensorial, motor and affect. Within each domain observers are asked to note the frequency of certain behaviours. For example, when observing ‘calling’ the observer is looking for ‘facial expressions, noises or gestures that seek to produce an affectionate response from the partner’.
A concern about the infant or the mother might be raised if a particular behaviour was never observed, perhaps showing a difficulty in relating, or was constantly observed, perhaps showing a defensive repetitiveness. The scales can be used to establish a thorough observational benchmark against which later changes can be compared.
Click here to see an example.
November 2015: diagnosing asthma this month, a synopsis of vitamin D deficiency as we go into the winter, a helpful cartoon around mental well-being and hypermobility demystified. All comments gratefully received!
Vitamin D deficiency in children with thanks to Dr Jini Haldar, paediatric registrar at Whipps Cross University Hospital.
Introduction
Vitamin D is an essential nutrient needed for healthy bones, and to control the amount of calcium in our blood. There is recent evidence that it may prevent many other diseases. There are many different recommendations for the prevention, detection and treatment of Vitamin D deficiency in the UK. The one outlined below is what we tend to do at Whipps Cross Hospital.
Prevention
The Department of Health and the Chief Medical Officers recommend a dose of 7-8.5 micrograms (approx. 300 units) for all children from six months to five years of age. This is the dose that the NHS ‘Healthy Start’ vitamin drops provide. The British Paediatric and Adolescent Bone Group’s recommendation is that exclusively breastfed infants receive Vitamin D supplements from soon after birth. Adverse effects of Vitamin D overdose are rare but care should be taken with multivitamin preparations as Vitamin A toxicity is a concern. Multivitamin preparations often contain a surprisingly low dose of Vitamin D.
Indications for measurement of vitamin D
1. Symptoms and signs of rickets/osteomalacia
2. Symptoms and signs of muscle weakness
3. Abnormal bone profile or x-rays
4. Disorders impacting on vitamin D metabolism
5. Children with bone disease in whom correcting vitamin D deficiency prior to specific treatment would be indicated:
Symptoms and signs in children of vitamin D deficiency
1. Infants: Seizures, tetany and cardiomyopathy
2. Children: Aches and pains: myopathy causing delayed walking; rickets with bowed legs, knock knees, poor growth and muscle weakness
3. Adolescents: Aches and pains, muscle weakness, bone changes of rickets or osteomalacia
Risk factors for reduced vitamin D levels include:
Management depends on the patient’s characteristics:
A. No risk factors
No investigations, lifestyle advice* and consider prevention of risk factors
B. Risk Factors Only
1. Children under the age of 5 years: Lifestyle advice* and vitamin D supplementation.
Purchase OTC or via Healthy Start
Under 1 year: 200 units vitamin D once daily
1 – 4 years: 400 units vitamin D once daily
2. Children 5 years and over – offer lifestyle advice*
C. Risk Factors AND Symptoms, Signs
Lifestyle advice*
Investigations:
Children can be managed in Primary Care as long as:
If further assessment is required consider referral to specialist. **
Patient’s family is likely to have similar risk of Vitamin D deficiency – consider investigation ant treatment if necessary.
1. Sunlight
Exposure of face, arms and legs for 5-10 mins (15-25 mins if dark pigmented skin) would provide good source of Vitamin D. In the UK April to September between 11am and 3pm will provide the best source of UVB. Application of sunscreen will reduce the Vitamin D synthesis by >95%. Advise to avoid sunscreen for the first 20-30 minutes of sunlight exposure. Persons wearing traditional black clothing can be advised to have sunlight exposure of face, arms and legs in the privacy of their garden.
2. Diet
Vitamin D can be obtained from dietary sources (salmon, mackerel, tuna, egg yolk), fortified foods (cow, soy or rice milk) and supplements. There are no plant sources that provide a significant amount of Vitamin D naturally.
Vitamin D levels, effects on health and management of deficiency
| level | effects |
management |
| < 25 nmol/l (10micrograms/l) | Deficient. Associated with rickets, osteomalacia | Treat with high dose vitamin D
Lifestyle advice AND vitamin D (ideally cholecalciferol) • 0 – 6 months: 3,000 units daily • 6 months – 12 yrs: 6,000 units daily • 12 – 18 yrs: 10,000 units daily |
| vitamin D 25 – 50 nmol/l (10 – 20micrograms/l | Insufficient and associated with disease risk | Over the counter (OTC) Vitamin D supplementation (and maintenance therapy following treatment for deficiency) should be sufficient.
• Lifestyle advice and vitamin D supplementation < 6 months: 200 – 400 units daily (200 units may be inadequate for breastfed babies) Over 6 months – 18 years: 400 – 800 units daily |
| 50 – 75 nmol/l (20 – 30micrograms/l) | Adequate | Healthy Lifestyle advice |
| > 75 nmol/l (30 micrograms/l) | Optimal Healthy | None |
Course length is 8 – 12 weeks followed by maintenance therapy.
Checking of levels again
As Vitamin D has a relatively long half-life levels will take approximately 6 months to reach a steady state after a loading dose or on maintenance therapy. Check serum calcium levels at 3 months and 6 months, and 25 – OHD repeat at 6 months. Review the need for maintenance treatment. NB: the Barts Health management protocol uses lower treatment doses for a minimum of 3 months and then there is no need for repeat blood tests in the majority of cases of children satisfying the criteria for management in primary care.
Serum 25 OHD after 3 months treatment Action
| level | action | review |
| >80nmol/ml | Recommend OTC prophylaxis and lifestyle advice | as required |
| 50 – 80 nmol/mL | Continue with current treatment dose | reassess in 3 months |
| < 50 nmol/mL | Increase dose or, in case of non-adherence/concern refer to secondary care. |
It is essential to check the child has a sufficient dietary calcium intake and that a maintenance vitamin D dose follows the treatment dose and is continued long term.
Follow-up:
Some recommend a clinical review a month after treatment starts, asking to see all vitamin and drug bottles. A blood test can be repeated then, if it is not clear that sufficient vitamin has been taken.
Current advice for children who have had symptomatic Vitamin D deficiency is that they continue a maintenance prevention dose at least until they stop growing. Dosing regimens vary and clinical evidence is weak in this area. The RCPCH has called for research to be conducted. The RCPCH advice on vitamin D is at http://www.rcpch.ac.uk/system/files/protected/page/vitdguidancedraftspreads%20FINAL%20for%20website.pdf
JINI HALDAR
– with thanks to Dr Joe Ward, paediatric registrar at Whipps Cross University Hospital.
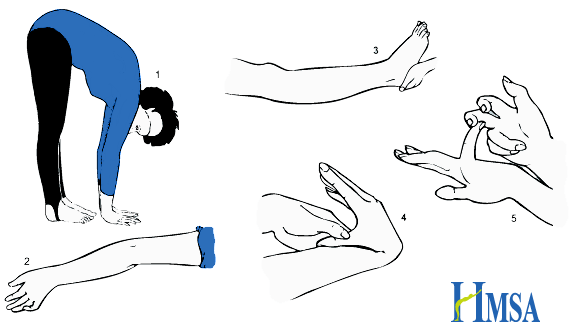 |
Picture from Hypermobility Syndromes Association
Hypermobility = synovial joints moving beyond normal range of movement.
Defined by the Beighton Score.: 1,2
Scores of 4 or above indicate Generalised Joint Hypermobility. May be asymptomatic, or associated with joint pain (exacerbated by exercise), dislocations and fatigue. Chronic pain often leads to muscle weakness. Other associations include dizziness and syncope and gastrointestinal problems such as chronic abdominal pain and constipation.
Physiotherapy and exercises to strengthen muscles around hypermobile joints provide the mainstay of treatment. Exercises to improve balance and coordination may also be helpful as proprioception may be impaired. Occupational therapy input may be beneficial.
The Brighton Criteria (NB: Brighton, not Beighton) is used in adults to diagnose Joint Hypermobility Syndrome. To make the diagnosis you need one of: two major criteria; one major and two minor criteria; four minor criteria; two minor criteria and one affected first degree relative. The presence of an underlying syndrome excludes the diagnosis. It is not yet validated in children.
Major Criteria:
Minor Criteria:
Connective tissue disorders associated with hypermobility should be excluded amongst children who meet the criteria for Joint Hypermobility Syndrome. These include but are not limited to:
Ehlers-Danlos Syndrome (http://www.ehlers-danlos.org/) – Heterogeneous group of disorders involving skin laxity, joint hypermobility, and vascular complications. Defined by the Villefranche Classification.
Marfan’s Syndrome (http://www.marfan.org/about/marfan) – Autosomal dominant connective tissue disorder. Typical features include characteristic facies, joint laxity, musculoskeletal problems (bone overgrowth and disproportionately long limbs), lens dislocation, and cardiovascular complications including aortic root dilatation.
Further information:
References:
1. Cattalini, M., Khubchandani, R. & Cimaz, R. When flexibility is not necessarily a virtue: a review of hypermobility syndromes and chronic or recurrent musculoskeletal pain in children. Pediatr. Rheumatol. Online J. 13, (2015).
2. Pacey, V., Tofts, L., Wesley, A., Collins, F. & Singh-Grewal, D. Joint hypermobility syndrome: a review for clinicians. J. Paediatr. Child Health 51, 373–380 (2015).