Peri-Orbital and Orbital Cellulitis in Children
With thanks to Dr Kat Smith, paediatric registrar and education fellow at King’s College Hospital….
The somewhat red, somewhat swollen eye is a relatively common presentation in children, and distinguishing between peri-orbital and orbital cellulitis hinges closely on an examination which can be difficult to perform in young children who cannot communicate pain on eye movement or subtle changes in vision.
Back to basics
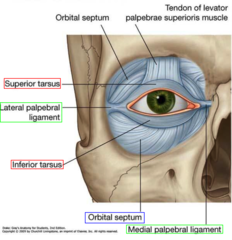
(Diagram above from quizlet.com)
The orbital septum is key in differentiating between peri-orbital and orbital cellulitis, and in dictating management. For those of us who haven’t thought about it since medical school, it is an extension of the periosteum of the frontal plate of the upper eyelid; a tough structure, where infection cannot pass from front to back unless the septum is breached by a sharp object. However, the orbital septum is not as thick and well developed in infants as it is in older children and adults, and so is not as effective a physical barrier in this age group.
Peri-orbital (or pre-septal) cellulitis is inflammation and infection of the eyelid soft tissue superficial and anterior to the orbital septum; the septum itself is not affected. Ocular function remains intact.
Orbital (or post-septal) cellulitis is infection of muscles and fat within the orbit, posterior to the orbital septum; the septum itself can be affected. It’s location in muscles and fat leads to associated ocular dysfunction.
What’s different in children?
Children are twice as likely to develop periorbital and orbital cellulitis in comparison to adults, and whilst in adults peri-orbital cellulitis is usually secondary to a superficial injury, children may develop it secondary to an occult underlying bacterial sinusitis (in particular, through the thin and porous ethmoid bone; there is often a history of recent URTI) or due to spread from another primary infection, such as pneumonia.
This difference in underlying aetiology means that in children a peri-orbital infection can rapidly progress to the much more concerning condition of orbital cellulitis, with the associated risk of rare but serious complications such as abscess formation, cavernous sinus thrombosis, intracranial abscess, and loss of vision.
Examination
The happy, well-looking child who is able to open their eye sufficiently for you to demonstrate normal light reflexes and see that they comfortably move their eyes in all planes more than likely has peri-orbital cellulitis; this will be most children. However, there are red flags that make orbital cellulitis a likely diagnosis and should prompt urgent referral to secondary care:
– Eyelid swelling such that the eye is not visible
– Toxic / systemically unwell
– CNS signs or symptoms
– Severe / persistent headache
– Pain on pressing the closed eyelid, indicating septal involvement
– Pain on eye movement, indicating involvement of muscle and / or fat
– Diplopia; older children should be able to describe “seeing double”, younger children may become unsteady when walking or struggle to grab objects
– Reduced visual acuity; the younger child may struggle to play with smaller / more “fiddly” toys
– Proptosis
– Ophthalmoplegia
– Absent light reflexes
– No improvement or worsening despite 48hrs oral antibiotics
– Neonatal age group (may be congenital dacryocystitis)
Management
Most children will be well, with mild-moderate swelling and erythema and no red flags; these children can initially be managed in the community, and most will not require later referral to secondary care.
Children with mild-moderate eyelid swelling, no significant erythema and an obvious cause – such as a chalazion or insect bite – do not have peri-orbital cellulitis, although they may need advice or treatment for the underlying cause such as warm compresses or anti-histamines.
Those with mild to moderate swelling, erythema and no obvious cause but no red flags are likely to have peri-orbital cellulitis and so require oral antibiotics; typically a 5-7 day course of co-amoxiclav is given, although this varies dependent on local microbiology guidance. Because of the underlying aetiology of peri-orbital cellulitis in children, parents should be advised that if children develop any red flag symptoms they require immediate medical review, and a GP review should be arranged for 48 hours’ time to ensure that symptoms have started to improve.
It can be unclear in young children if they have any red flags; if in doubt, refer to secondary care for review by ophthalmology, A&E, or paediatric teams. Even in secondary care it can be unclear, and children may be admitted simply for oral antibiotics and observation. ENT teams will also need to be involved if orbital cellulitis is suspected.
As above, children with any red flags are likely to have orbital cellulitis and will likely require admission to hospital for blood tests, cultures and IV antibiotics +/- imaging of the sinuses and orbits (although more extensive neuroimaging is indicated if there is a suspicion of cerebral infection).
References
“Children are twice as likely to develop periorbital and orbital cellulitis in comparison to adults”
Robinson A, Beech T, McDermott A, et al. Investigation and Management of adult periorbital or orbital cellulitis. J Laryngol Oto. 2007;121:545-7.
Bibliography:
BMJ Best Practice: Peri-orbital and orbital cellulitis. Available from http://bestpractice.bmj.com/best-practice/monograph/734.html
Clarke W. Periorbital and orbital cellulitis in children. Paediatr Child Health. 2004;9(7):471-2
The College of Optometrists. Clinical Management Guidelines. Cellulitis, preseptal and orbital. Available from http://www.college-optometrists.org/en/utilities/document-summary.cfm/docid/25FDE60B-E41D-4212-8AB02819A83E72E1