March 2016: a few odds and ends on asthma this month and assessing a child in an acute exacerbation, Childline survey, Meningococcus W and paediatric neck lumps. Do leave comments below:
Category Archives: For Emergency Departments
February 2016
Stepwise management of asthma this month. Plus some information on infant mental health, paediatric airways and a few more sites on internet safety. Do leave comments below.
Welcome to January 2016
January 2016 newsletter continues on the theme of asthma and covers internet safety, IDA and early weight loss in breastfed babies. Do leave comments below:
November 2015 newsletter
November 2015: diagnosing asthma this month, a synopsis of vitamin D deficiency as we go into the winter, a helpful cartoon around mental well-being and hypermobility demystified. All comments gratefully received!
How to use the Beighton score
Hypermobility
– with thanks to Dr Joe Ward, paediatric registrar at Whipps Cross University Hospital.
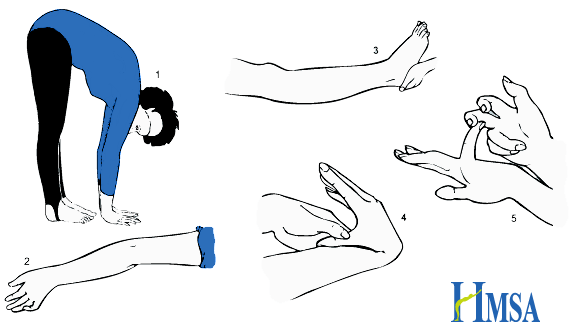 |
Picture from Hypermobility Syndromes Association
Hypermobility = synovial joints moving beyond normal range of movement.
Defined by the Beighton Score.: 1,2
- Ability to touch palms flat to floor with knees straight (one point)
- Elbow extension >10° (one point for each side)
- Knee extension >10° (one point for each side)
- Ability to touch thumb to forearm (one point for each side)
- Fifth finger metocarpalphalageal joint extension >90° (one point for each side)
Scores of 4 or above indicate Generalised Joint Hypermobility. May be asymptomatic, or associated with joint pain (exacerbated by exercise), dislocations and fatigue. Chronic pain often leads to muscle weakness. Other associations include dizziness and syncope and gastrointestinal problems such as chronic abdominal pain and constipation.
Physiotherapy and exercises to strengthen muscles around hypermobile joints provide the mainstay of treatment. Exercises to improve balance and coordination may also be helpful as proprioception may be impaired. Occupational therapy input may be beneficial.
The Brighton Criteria (NB: Brighton, not Beighton) is used in adults to diagnose Joint Hypermobility Syndrome. To make the diagnosis you need one of: two major criteria; one major and two minor criteria; four minor criteria; two minor criteria and one affected first degree relative. The presence of an underlying syndrome excludes the diagnosis. It is not yet validated in children.
Major Criteria:
- Beighton Score >3
- Arthralgia > 3 months in four or more joints
Minor Criteria:
- Beighton Score 1-3,
- Arthralgia > 3 months in one joint, backpain, or spondylosis / spondylolysis / spondylolisthesis
- Dislocation or subluxation in more than one joint, or in one joint repeatedly
- Three or more soft tissue lesions (e.g epicondylitis, tenosynovitis, bursitis)
- Marfanoid habitus
- Skin striae
- Ocular signs (e.g drooping eyelids, myopia, antimongoloid slant)
- Varicose veins, hernia, uterine or rectal prolapse
- Mitral valve prolapse
Connective tissue disorders associated with hypermobility should be excluded amongst children who meet the criteria for Joint Hypermobility Syndrome. These include but are not limited to:
Ehlers-Danlos Syndrome (http://www.ehlers-danlos.org/) – Heterogeneous group of disorders involving skin laxity, joint hypermobility, and vascular complications. Defined by the Villefranche Classification.
Marfan’s Syndrome (http://www.marfan.org/about/marfan) – Autosomal dominant connective tissue disorder. Typical features include characteristic facies, joint laxity, musculoskeletal problems (bone overgrowth and disproportionately long limbs), lens dislocation, and cardiovascular complications including aortic root dilatation.
Further information:
References:
1. Cattalini, M., Khubchandani, R. & Cimaz, R. When flexibility is not necessarily a virtue: a review of hypermobility syndromes and chronic or recurrent musculoskeletal pain in children. Pediatr. Rheumatol. Online J. 13, (2015).
2. Pacey, V., Tofts, L., Wesley, A., Collins, F. & Singh-Grewal, D. Joint hypermobility syndrome: a review for clinicians. J. Paediatr. Child Health 51, 373–380 (2015).
October 2015 newsletter
We have seen a lot of cases of scarlet fever this year so thanks to Dr Lock for his text box this month on recognising and managing this strep infection. Comprehensive information on paediatric dizziness from Mr Sharma, ENT registrar, and a bit about asthma in schools and some of my own CPD on birthmarks caused by a Mum whose view that the internet knew more than me was a little unsettling – for a while. We have all been there, I’m sure.
Do leave comments below.
September 2015 uploaded
September 2015: ENT feature this month – quinsy, Part 2 of the NICE guideline summary on bronchiolitis, information about a domestic violence campaign, self help books for children and a round up of topics to get you started if you are new to paediatric practice. Do leave comments below.
August 2015
August 2015: ENT feature this month – acute mastoiditis, PVL producing staph from the dermatology team, Henoch Schonlein purpura – long term management and follow up and Part 1 of the NICE guideline summary on bronchiolitis. Just in time for the RSV season….
Do leave comments below:
July 2015 being uploaded on a Sunday in honour of the Right Honourable Jeremy Hunt
Chest pain this month – which is very rarely cardiac in the paediatric population, early recognition of various childhood cancers, links to some drug and alcohol support groups, paediatric drooling. Do leave comments.
June 2015 published
Gianotti Crosti this month, updated “Working Together” safeguarding document, epistaxis and malaria. Also links to a few other useful documents recently uploaded to the Primary Care Guidelines part of the website, with thanks to Redbridge and West Suffolk. All comments welcome.